Diabetes mellitus, a general metabolic disease attacking millions of people worldwide, is a great challenge in the modern world of medicine. At the heart of this test are beta cells, which performs an important role in regulating the delicate balance of blood sugar medications. This article analyzes the complicated transaction between beta cells and diabetes and their fundamental job in keeping up with metabolic equilibrium. From their basic capabilities in insulin blend and glucose detecting to their fragile connections with the resistant framework and ecological elements, beta cells go about as guardians of glucose. As we dig further into their space, understanding the significant outcomes of beta cell brokenness becomes vital for creating powerful systems for overseeing and forestalling diabetes.
Beta cells and diabetes
Two types of Diabetes.
Type 1 Diabetes: This insulin-dependent situation is caused by an assault on and collapse of the pancreatic beta cells that give insulin by the resolute framework. This creates a shortage of insulin to be generated, which raises blood glucose levels. Long-term insulin therapy is called for glucose handling in people with Type 1 diabetes.
Type 2 Diabetes: Type 2 diabetes is portrayed by insulin opposition, where the body’s cells become insensitive to insulin, and the pancreas may not produce enough insulin to compensate.Way of life parts like weight and less than stellar eating routine add to its turn of events. Treatment incorporates way of life changes, prescriptions, and at times insulin treatment to oversee glucose levels.
READ ALSO :- Selecting the Ideal Rehabilitation Center: Key Considerations
Role of beta cells
They produce insulin at elevated blood glucose concentrations to regulate blood sugar levels. Besides this function, they also take sugar after meals by producing insulin for energy or storage so as to maintain normal levels of glycemia within an individual’s body systems.
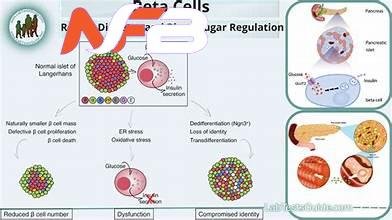
Understanding Beta Cell Activity: Inside the pancreas are Langerhans’ islets, where beta cells—the most crucial agents of glucose homeostasis—reside. They mainly sense variations in blood sugar amounts and react by producing insulin, a hormone that helps drive glucose into cells for energy or storage purposes. If this finely tuned procedure is interrupted, it leads to hyperglycemia or hypoglycemia conditions.
Revealing the Two Faces of Diabetes: Diabetes can be categorized into two broad types with different implications for beta cell functioning. In type 1 diabetes mellitus, an immune-independent strike to fall and approach pancreatic beta cells, leading to insulin shortage. On the other hand, type 2 diabetes mellitus shows from a combination of peripheral tissue resistance to insulin and compromised function of beta cells. All these incidences disrupt the fine balance maintained by beta cells, resulting in uncontrolled blood sugars.
Instructing and connecting with patients: The most fundamental step is enabling people with diabetes to play a functioning job in their own consideration. Schooling drives pointed toward cultivating comprehension of the elements of the beta cells in the body; the pathogenesis of diabetes mellitus; and accessible remedial choices that permit patients to make informed choices on how best to deal with their sickness.
Glucose Detection: Beta cells have a specific glucose-detecting apparatus that permits them to identify even unpretentious changes in glucose levels. This intense responsiveness empowers beta cells to start insulin discharge expeditiously because of rising glucose fixations, forestalling unreasonable spikes in glucose.
Insulin Discharge Elements: Beta cells display striking adaptability in adjusting the magnitude and energy of insulin emission in light of the predominant metabolic requests. Quick delivery pools of insulin put away inside beta cells work with quick reactions to postprandial glucose floods, while supported insulin discharge guarantees delayed glucose take-up during times of expanded energy consumption.
Counterregulatory Chemical Guideline: Past insulin emission, beta cells assume a critical role in planning the discharge of counterregulatory chemicals, for example, glucagon, which acts to raise glucose levels. This sensitive transaction between insulin and glucagon guarantees dynamic changes in glucose accessibility, keeping up with metabolic harmony in different physiological states.
Metabolic Homeostasis: Beta cells add to the support of metabolic homeostasis by coordinating the harmony between glucose take-up, usage, and capacity in fringe tissues. Through insulin-interceded flagging pathways, beta cells advance glucose take-up by skeletal muscle and fat tissue, hinder hepatic glucose creation, and work with glycogen union, in this manner adjusting fundamental glucose levels.
Neuroendocrine Correspondence: Beta cells participate in bidirectional correspondence with the focal sensory system (CNS) and fringe neuroendocrine organs to coordinate metabolic prompts and direct fundamental reactions. Synapses, neuropeptides, and hormonal signs radiating from the CNS and extrapancreatic tissues tweak beta cell capability, adjusting insulin emission as per metabolic requests and natural improvements.
Roles of Beta Cells in Diabetes: Doctors’s Quotes
Here is a quotation about the role of beta cells in diabetes.
Beta Cell Brokenness as a Driver of Sickness Movement: Dr. Daniel J. Drucker, a noticeable endocrinologist, stresses the focal part of beta cell brokenness in the pathogenesis of type 2 diabetes. He states that while insulin resistance starts the illness cycle, beta cell disappointment eventually decides infection movement, highlighting the basic significance of protecting beta cell capability.
Beta Cell Versatility and Regenerative Potential: Dr. Pedro L. Herrera, a trailblazer in the field of beta cell science, has explored the regenerative limit of beta cells and their true capacity for renewing lost or useless cells in diabetes. His exploration has uncovered the presence of idle begetter cells inside the pancreas fit for separating into practical beta cells, offering expected regenerative treatments.
Beta Cell Crosstalk with Resistant Cells: Dr. Matthias von Herrath, a specialist in immune system diabetes, has investigated the powerful transaction between beta cells and resistant cells with regard to Type 1 diabetes. He highlights the bidirectional correspondence between beta cells and insusceptible effectors, wherein beta cell-determined antigens trigger immune system reactions while immunomodulatory factors emitted by beta cells control resistant resilience and aggravation.
Natural Effects on Beta Cell Capability: Dr. Barbara E. Corkey, a recognized specialist in metabolic illnesses, has examined the effect of ecological variables on beta cell capability and weakness in diabetes medicine. Her work features the job of dietary supplements, oxidative pressure, and fiery arbiters in regulating beta cell digestion and insulin emission, highlighting the complicated transaction between hereditary inclination and natural triggers in diabetes pathogenesis.
READ ALSO :- Exploring “wellhealthorganic.com/easily-remove-dark-spots-lemon-juice”
Conclusion
All in all, the perplexing transaction between beta cells and diabetes uncovers a charming adventure of cell guardianship in the domain of metabolic guidelines. As the overseers of glucose homeostasis, beta cells coordinate an ensemble of insulin discharges, tweaking their reactions to fluctuating metabolic requests and ecological signs. From their urgent jobs in glucose detection and insulin discharge to their nuanced communications with resistant effectors and metabolic substrates, beta cells arise as the key part of diabetes pathophysiology. The steady attack on beta cells in Type 1 diabetes, intensified by the tricky decrease in capability found in Type 2 diabetes, highlights the earnestness of safeguarding beta cell well-being to prevent illness movement.














Leave a Reply